Understanding Endometrial Cancer: Diagnosis, Treatment & Support
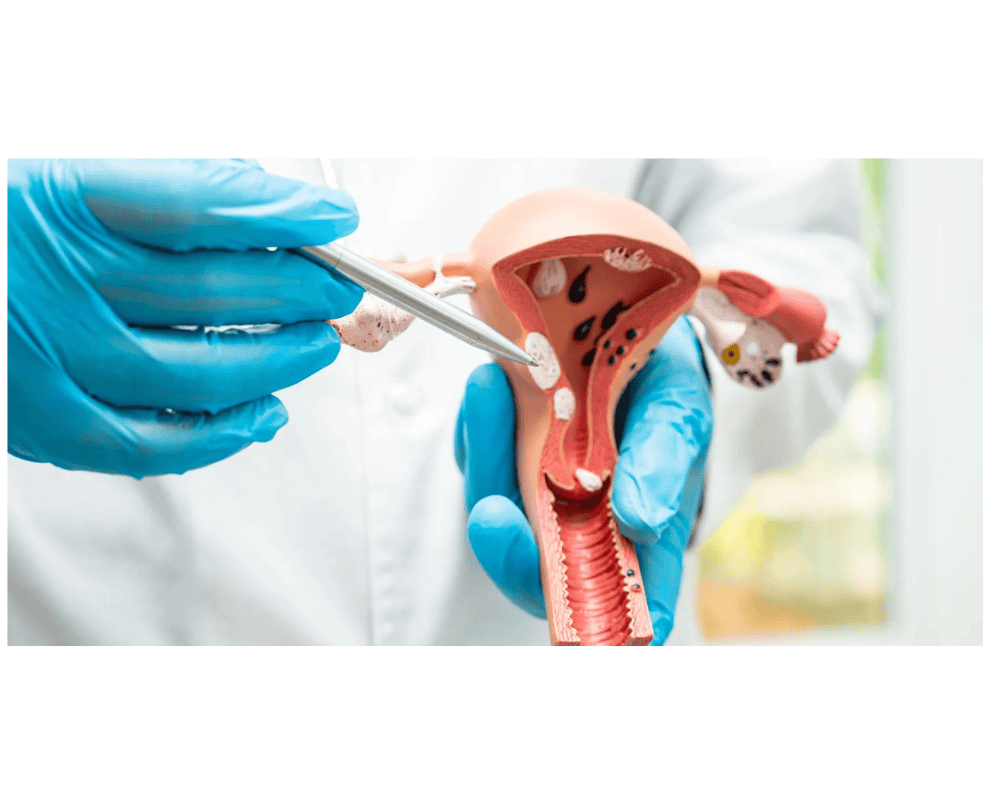
Endometrial carcinoma, also known as uterine cancer, is the most common cancer of the female reproductive system. It originates in the lining of the uterus, called the endometrium. This type of cancer typically affects women after menopause, but it can occur earlier. Endometrial carcinoma is often detected at an early stage due to abnormal vaginal bleeding, which leads women to seek medical attention. Early detection greatly improves the chances of successful treatment.
Endometrial carcinoma, also known as uterine cancer, is the most common cancer of the female reproductive system. It originates in the lining of the uterus, called the endometrium. This type of cancer typically affects women after menopause, but it can occur earlier. Endometrial carcinoma is often detected at an early stage due to abnormal vaginal bleeding, which leads women to seek medical attention. Early detection greatly improves the chances of successful treatment.
Risk Factors
Several factors can increase the risk of developing endometrial carcinoma:
- Age: Most cases occur in women over the age of 50.
- Hormonal Imbalance: Conditions like polycystic ovarian syndrome (PCOS) or hormone replacement therapy, particularly estrogen therapy without progesterone, can raise the risk.
- Obesity: Excess body fat can lead to increased estrogen levels, heightening the risk.
- Diabetes: Women with diabetes may be more susceptible.
- Family History: A family history of endometrial, ovarian, or colon cancer can increase the risk.
- Genetic Conditions: Lynch syndrome, a hereditary cancer syndrome, significantly raises the likelihood of endometrial cancer.
- Tamoxifen: Long-term use of the breast cancer drug tamoxifen may slightly raise the risk.
Several factors can increase the risk of developing endometrial carcinoma:
- Age: Most cases occur in women over the age of 50.
- Hormonal Imbalance: Conditions like polycystic ovarian syndrome (PCOS) or hormone replacement therapy, particularly estrogen therapy without progesterone, can raise the risk.
- Obesity: Excess body fat can lead to increased estrogen levels, heightening the risk.
- Diabetes: Women with diabetes may be more susceptible.
- Family History: A family history of endometrial, ovarian, or colon cancer can increase the risk.
- Genetic Conditions: Lynch syndrome, a hereditary cancer syndrome, significantly raises the likelihood of endometrial cancer.
- Tamoxifen: Long-term use of the breast cancer drug tamoxifen may slightly raise the risk.
Symptoms
Common signs and symptoms of endometrial carcinoma include:
- Abnormal vaginal bleeding, especially after menopause
- Pelvic pain or discomfort
- Pain during intercourse
- Unexplained weight loss
- Vaginal discharge that may be watery or tinged with blood
If these symptoms persist or worsen, it is essential to consult a healthcare professional for further evaluation.
Common signs and symptoms of endometrial carcinoma include:
- Abnormal vaginal bleeding, especially after menopause
- Pelvic pain or discomfort
- Pain during intercourse
- Unexplained weight loss
- Vaginal discharge that may be watery or tinged with blood
If these symptoms persist or worsen, it is essential to consult a healthcare professional for further evaluation.
Diagnosis
Endometrial carcinoma can be diagnosed using a variety of methods, including:
- Pelvic Examination: A physical examination of the pelvic area to check for any abnormalities.
- Transvaginal Ultrasound: An imaging test that uses sound waves to create images of the uterus and detect changes in the endometrium.
- Endometrial Biopsy: A procedure where a small tissue sample is taken from the endometrium to examine for cancerous cells.
- Dilation and Curettage (D&C): A more invasive procedure that allows for a larger tissue sample to be collected for analysis.
- Imaging Tests: CT scans, MRIs, or PET scans may be used to determine if the cancer has spread.
Endometrial carcinoma can be diagnosed using a variety of methods, including:
- Pelvic Examination: A physical examination of the pelvic area to check for any abnormalities.
- Transvaginal Ultrasound: An imaging test that uses sound waves to create images of the uterus and detect changes in the endometrium.
- Endometrial Biopsy: A procedure where a small tissue sample is taken from the endometrium to examine for cancerous cells.
- Dilation and Curettage (D&C): A more invasive procedure that allows for a larger tissue sample to be collected for analysis.
- Imaging Tests: CT scans, MRIs, or PET scans may be used to determine if the cancer has spread.
Treatment Options
- Surgery: The primary treatment for endometrial carcinoma is surgery, usually involving a hysterectomy (removal of the uterus) along with the removal of the ovaries and fallopian tubes. In some cases, lymph nodes may also be removed to check for cancer spread.
- Radiation Therapy: Radiation may be used post-surgery or as a primary treatment if surgery is not an option. It helps to destroy remaining cancer cells.
- Hormone Therapy: For women with advanced endometrial cancer, hormone therapy using progestins may slow the growth of cancer cells.
- Chemotherapy: Chemotherapy may be recommended for more advanced stages of the disease or if the cancer returns. It is often used in combination with radiation or surgery.
- Surgery: The primary treatment for endometrial carcinoma is surgery, usually involving a hysterectomy (removal of the uterus) along with the removal of the ovaries and fallopian tubes. In some cases, lymph nodes may also be removed to check for cancer spread.
- Radiation Therapy: Radiation may be used post-surgery or as a primary treatment if surgery is not an option. It helps to destroy remaining cancer cells.
- Hormone Therapy: For women with advanced endometrial cancer, hormone therapy using progestins may slow the growth of cancer cells.
- Chemotherapy: Chemotherapy may be recommended for more advanced stages of the disease or if the cancer returns. It is often used in combination with radiation or surgery.
Newer Treatment Options
Recent advancements in the treatment of endometrial carcinoma include:
- Targeted Therapy: Drugs that target specific molecules in cancer cells to inhibit their growth. For example, inhibitors of the PI3K/AKT/mTOR pathway have shown promise in clinical trials for endometrial cancer.
- Minimally Invasive Surgery: Laparoscopic and robotic-assisted surgeries allow for less invasive procedures with quicker recovery times, reduced pain, and minimal scarring.
Recent advancements in the treatment of endometrial carcinoma include:
- Targeted Therapy: Drugs that target specific molecules in cancer cells to inhibit their growth. For example, inhibitors of the PI3K/AKT/mTOR pathway have shown promise in clinical trials for endometrial cancer.
- Minimally Invasive Surgery: Laparoscopic and robotic-assisted surgeries allow for less invasive procedures with quicker recovery times, reduced pain, and minimal scarring.
Role of Immunotherapy
Immunotherapy, which boosts the body’s immune system to fight cancer, is an emerging option for treating advanced or recurrent endometrial carcinoma. The most commonly used immunotherapy in endometrial cancer is checkpoint inhibitors like pembrolizumab, which targets the PD-1/PD-L1 pathway to enhance immune response against cancer cells. This approach is particularly effective for tumors with high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR), making it a personalized treatment option based on tumor genetics.
Immunotherapy, which boosts the body’s immune system to fight cancer, is an emerging option for treating advanced or recurrent endometrial carcinoma. The most commonly used immunotherapy in endometrial cancer is checkpoint inhibitors like pembrolizumab, which targets the PD-1/PD-L1 pathway to enhance immune response against cancer cells. This approach is particularly effective for tumors with high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR), making it a personalized treatment option based on tumor genetics.
Why Choose ID Cancer Center for Endometrial Cancer?
The ID Cancer Center offers comprehensive and cutting-edge care for patients diagnosed with endometrial carcinoma. Here are key reasons why choosing ID Cancer Center ensures the highest standard of treatment:
The ID Cancer Center offers comprehensive and cutting-edge care for patients diagnosed with endometrial carcinoma. Here are key reasons why choosing ID Cancer Center ensures the highest standard of treatment:
1. Expert Team of Oncologists
At ID Cancer Center, a multidisciplinary team of highly experienced specialists, including gynecologic oncologists, radiation oncologists, and medical oncologists, collaborates to deliver personalized treatment plans. Our team is equipped to handle both early-stage and advanced endometrial cancer cases.
At ID Cancer Center, a multidisciplinary team of highly experienced specialists, including gynecologic oncologists, radiation oncologists, and medical oncologists, collaborates to deliver personalized treatment plans. Our team is equipped to handle both early-stage and advanced endometrial cancer cases.
2. Advanced Diagnostic Tools
Early and accurate diagnosis is critical in endometrial carcinoma. The ID Cancer Center utilizes state-of-the-art diagnostic technology, including transvaginal ultrasounds, advanced imaging (MRI, CT, PET), and genetic testing for conditions like Lynch syndrome, to assess the full extent of the cancer and plan the most effective treatment.
Early and accurate diagnosis is critical in endometrial carcinoma. The ID Cancer Center utilizes state-of-the-art diagnostic technology, including transvaginal ultrasounds, advanced imaging (MRI, CT, PET), and genetic testing for conditions like Lynch syndrome, to assess the full extent of the cancer and plan the most effective treatment.
3. Comprehensive Treatment Options
Our center offers a wide range of treatment options, from conventional surgery and radiation therapy to cutting-edge treatments like:
- Minimally Invasive Surgery: Robotic-assisted and laparoscopic procedures that ensure quicker recovery with minimal scarring.
- Targeted Therapy: Personalized treatment using drugs that focus on the specific genetic makeup of your tumor.
- Immunotherapy: Leveraging the body’s immune system to combat cancer, especially for patients with advanced or recurrent cases.
- Hormone Therapy: For hormone-sensitive cancers, we offer the latest hormone therapies that can slow the growth of cancer cells.
Our center offers a wide range of treatment options, from conventional surgery and radiation therapy to cutting-edge treatments like:
- Minimally Invasive Surgery: Robotic-assisted and laparoscopic procedures that ensure quicker recovery with minimal scarring.
- Targeted Therapy: Personalized treatment using drugs that focus on the specific genetic makeup of your tumor.
- Immunotherapy: Leveraging the body’s immune system to combat cancer, especially for patients with advanced or recurrent cases.
- Hormone Therapy: For hormone-sensitive cancers, we offer the latest hormone therapies that can slow the growth of cancer cells.
4. Focus on Newer Treatment Modalities
ID Cancer Center is at the forefront of innovative cancer treatments, offering access to cutting-edge clinical trials and the latest therapies, such as:
- Checkpoint inhibitors: Immunotherapy drugs that have shown excellent results for specific types of endometrial cancer, like those with mismatch repair deficiencies.
- Proton Therapy: A highly precise form of radiation therapy that minimizes damage to surrounding healthy tissue while effectively targeting cancer cells.
ID Cancer Center is at the forefront of innovative cancer treatments, offering access to cutting-edge clinical trials and the latest therapies, such as:
- Checkpoint inhibitors: Immunotherapy drugs that have shown excellent results for specific types of endometrial cancer, like those with mismatch repair deficiencies.
- Proton Therapy: A highly precise form of radiation therapy that minimizes damage to surrounding healthy tissue while effectively targeting cancer cells.
5. Holistic Patient Care
At ID Cancer Center, we believe in treating not just the disease but the whole person. Our comprehensive care approach includes:
- Emotional and psychological support through counseling services.
- Nutritional guidance to help patients maintain strength and well-being during treatment.
- Rehabilitation and survivorship programs designed to help patients recover and regain their quality of life after treatment.
At ID Cancer Center, we believe in treating not just the disease but the whole person. Our comprehensive care approach includes:
- Emotional and psychological support through counseling services.
- Nutritional guidance to help patients maintain strength and well-being during treatment.
- Rehabilitation and survivorship programs designed to help patients recover and regain their quality of life after treatment.
6. Personalized Care and Support
We tailor our treatment plans to the individual, considering each patient's specific medical history, genetic profile, and preferences. The center also provides dedicated patient support services to guide individuals through every step of their cancer journey, from diagnosis to recovery.
We tailor our treatment plans to the individual, considering each patient's specific medical history, genetic profile, and preferences. The center also provides dedicated patient support services to guide individuals through every step of their cancer journey, from diagnosis to recovery.
7. Convenient and Coordinated Care
The ID Cancer Center ensures a seamless experience, coordinating all aspects of care under one roof, from diagnostics and surgery to radiation and chemotherapy. Our patient navigators streamline the process, making sure patients receive timely care without delays.
The ID Cancer Center ensures a seamless experience, coordinating all aspects of care under one roof, from diagnostics and surgery to radiation and chemotherapy. Our patient navigators streamline the process, making sure patients receive timely care without delays.
8. Commitment to Research and Innovation
Our center is deeply involved in research and clinical trials, ensuring that patients have access to the latest breakthroughs in endometrial cancer treatment. By participating in cutting-edge research, we continually advance the care we provide, making us a leader in cancer treatment innovation.
Our center is deeply involved in research and clinical trials, ensuring that patients have access to the latest breakthroughs in endometrial cancer treatment. By participating in cutting-edge research, we continually advance the care we provide, making us a leader in cancer treatment innovation.
Conclusion
Choosing ID Cancer Center means entrusting your care to a world-class institution with a proven track record in the diagnosis and treatment of endometrial carcinoma. With our expert team, advanced technologies, and commitment to holistic care, we provide every patient with the best chance of a successful outcome and a better quality of life.
Choosing ID Cancer Center means entrusting your care to a world-class institution with a proven track record in the diagnosis and treatment of endometrial carcinoma. With our expert team, advanced technologies, and commitment to holistic care, we provide every patient with the best chance of a successful outcome and a better quality of life.
